Untreated rabies is almost always fatal but 100% vaccine-preventable4,5
How is Rabies Transmitted?
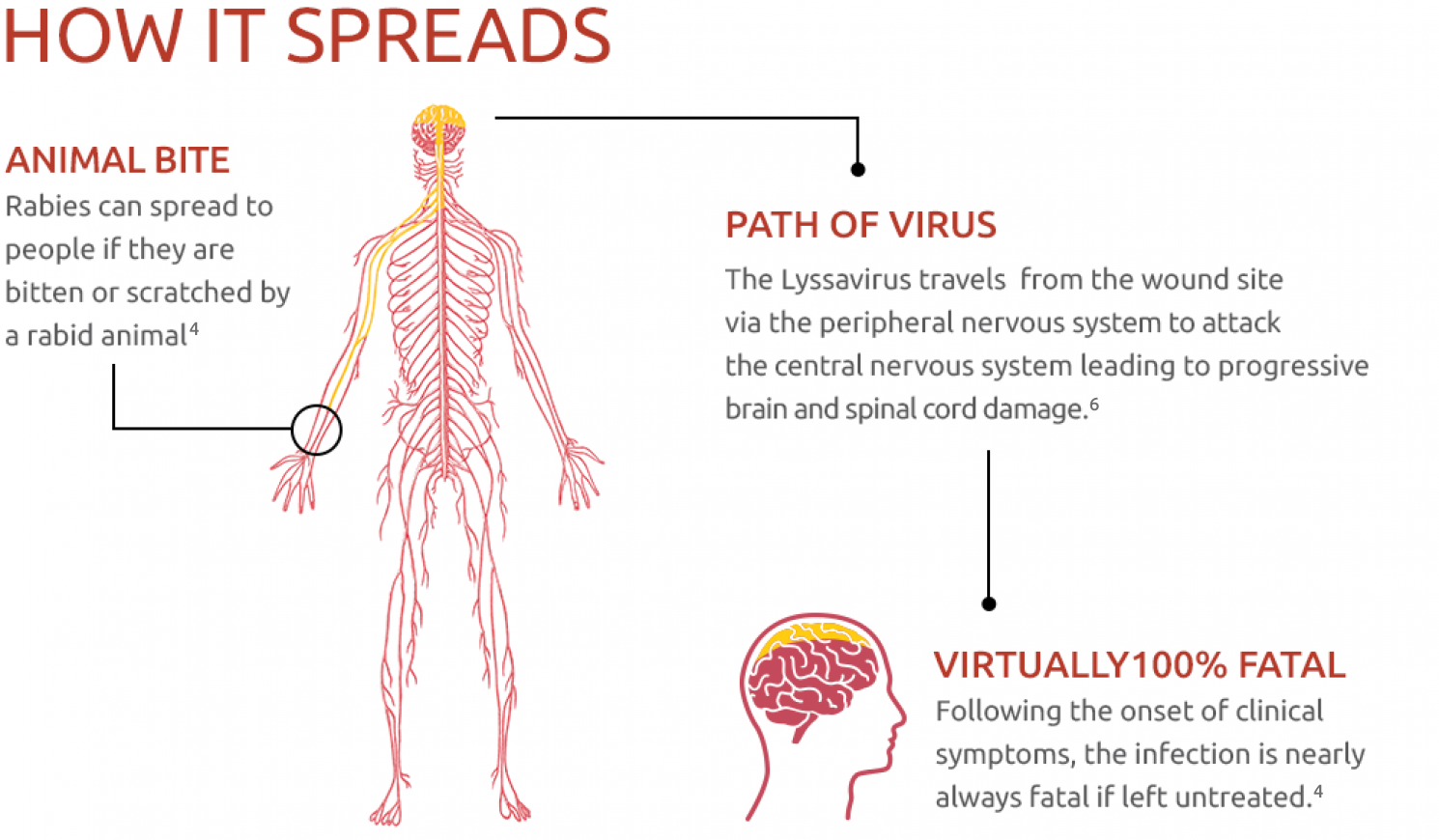
- Rabies is transmitted in the saliva of rabid animals and generally enters the body when individuals are exposed to virus-laden saliva via scratches or bites4
Animals that Transmit Rabies
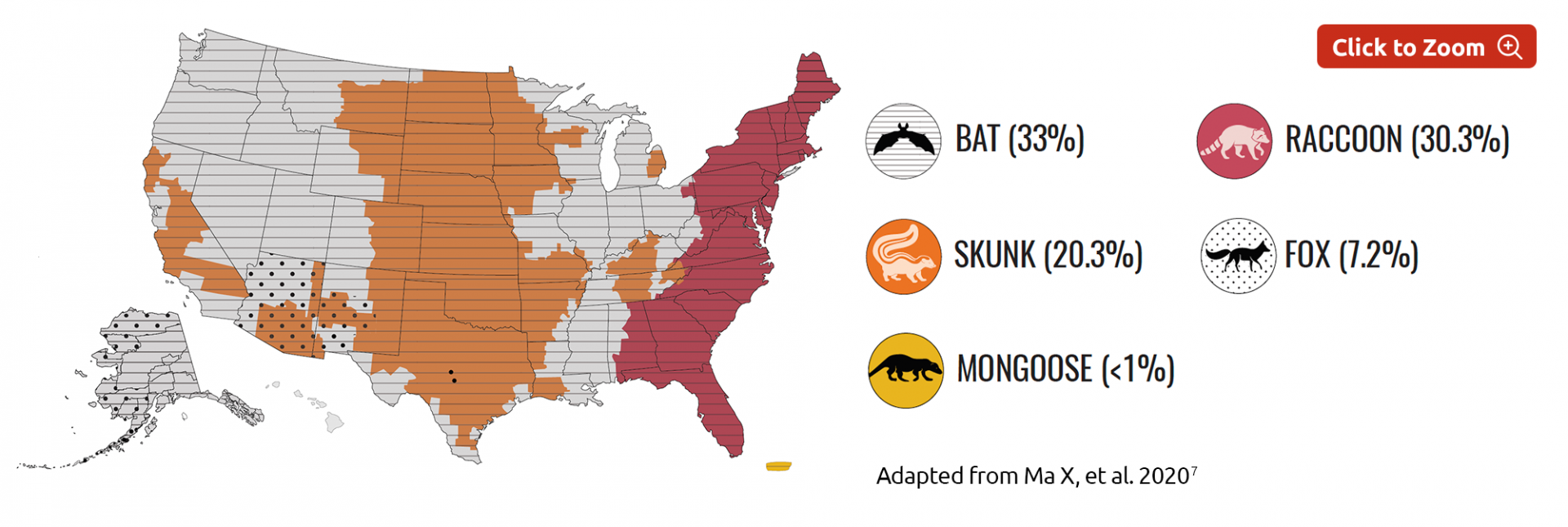
Globally, 99% of human rabies deaths are caused by dogs.4
- In the Americas, bats are now the major source of human rabies deaths as dog-mediated transmission has mostly been eliminated in this region4
- Other common carriers include Racoon, Monkey, Fox, Mongoose and Cat2
Common Carriers
Rabies in the US
Wild animals accounted for 92.7% of reported cases of rabies in the US in 20187
Who is at Risk?
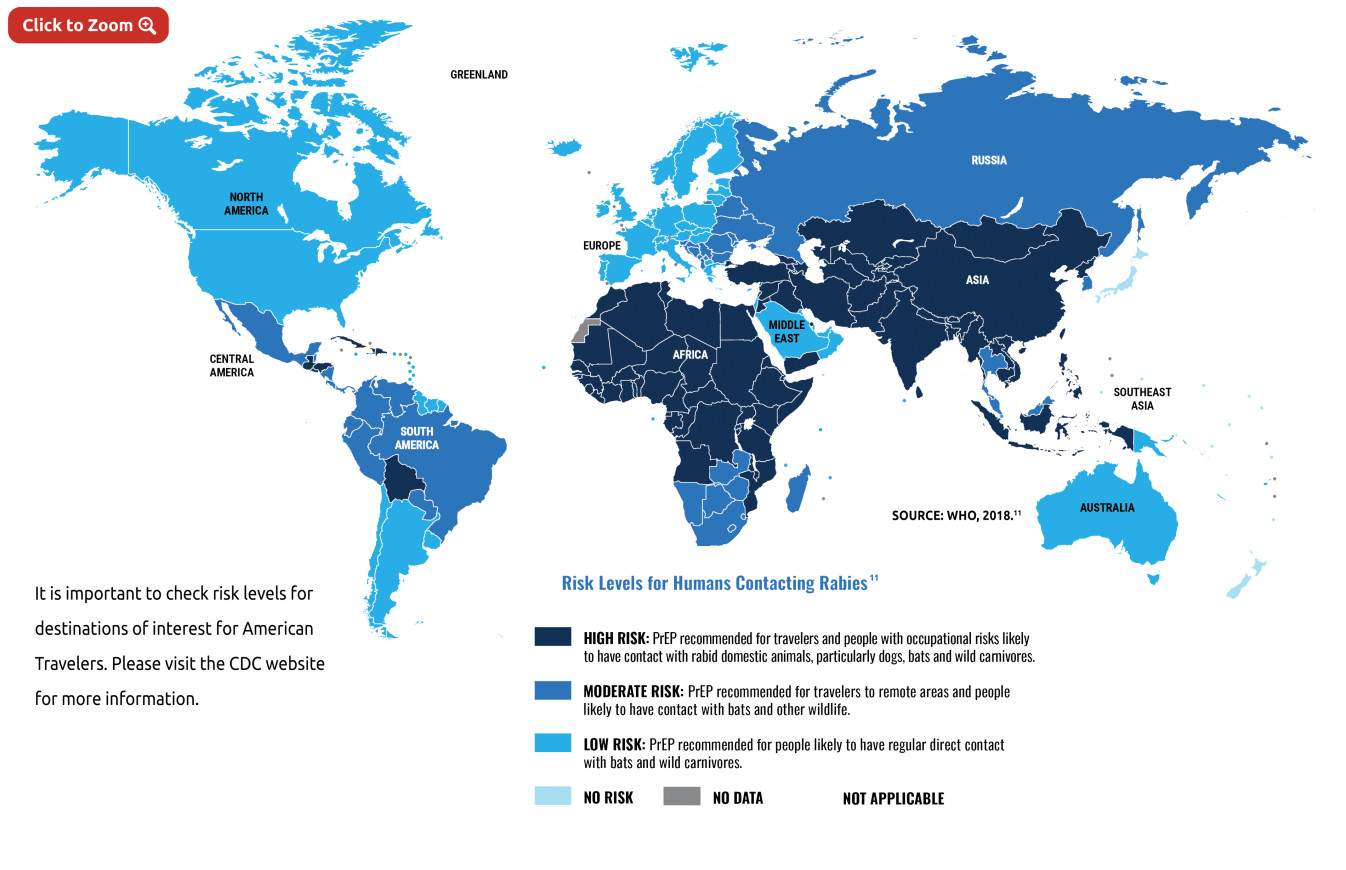
Veterinarians, animal handlers, wildlife officers in areas where animal rabies is enzootic, certain laboratory workers, and persons spending time in foreign countries where rabies is endemic are at higher risk of rabies exposure.8
Pre-exposure vaccination should be offered to persons in high-risk groups and whose activities bring them into contact with potentially rabid dogs, cats, foxes, skunks, bats, or other species at risk of having rabies.8
International travelers might be candidates for pre-exposure vaccination if they are likely to come in contact with animals in areas where dog rabies is enzootic and immediate access to appropriate medical care, including biologics, might be limited.8
Finally, immunization should also be considered for children living in, or visiting remote areas with a high rabies exposure. As they play with animals, they may receive more severe bites, or may not report bites.4,9
Rabies pre-exposure prophylaxis guide10
|
Risk Category
|
Nature of Risk
|
Typical Population
|
Pre-exposure Recommendations
|
|
Continuous
|
Virus present continuously
Specific exposures likely to go unrecognized
|
Rabies research laboratory workers
Rabies biologics production workers
|
Primary course. Serologic testing every 6 months; booster vaccination if antibody titer is below acceptable level.
|
|
Frequent
|
Exposure usually episodic, with source recognized, but exposure also might be unrecognized
|
Rabies diagnostic lab workers
Spelunkers
Veterinarians and staff
Animal-control and wildlife workers in rabies-enzootic areas
Persons who frequently handle bats
|
Primary course. Serologic testing every 2 years; booster vaccination if antibody titer is below acceptable level.
|
|
Infrequent
|
Exposure nearly always episodic with source recognized
|
Veterinarians and terrestrial animal-control workers in areas where rabies is uncommon to rare. Veterinary students
Travelers visiting areas where rabies is enzootic and immediate access to appropriate medical care including biologics is limited
|
Primary course. No serologic testing or booster vaccination.
|
|
Rare
|
Exposure always episodic with source recognized
|
U.S. residents, including persons living in rabies-epizootic areas.
|
No vaccination necessary.
|
Adapted from: https://www.cdc.gov/rabies/specific_groups/travelers/pre-exposure_vaccinations.html
Clinical Manifestations of Rabies
- Infection with this neurotropic virus results in neurological and psychological manifestations4
- The incubation period is usually 2–3 months, but can vary from 1 week to 1 year depending upon factors such as the location of virus entry and viral load4
- Initial symptoms include a fever with pain and unusual or unexplained tingling, pricking, or paraesthesia at the wound site4
- As the virus spreads to the central nervous system, there is paralysis and coma, and finally death4
|
Furious rabies4
|
Paralytic rabies4
|
|
~80% of rabies cases
|
~20% of rabies cases
|
|
Characterised by signs of CNS irritation:
-
Hyperactivity
-
Excitable behaviour
-
Hydrophobia
-
Aerophobia
|
Characterised by weakness and paralysis:
|
|
Rapidly progressing disease, with death due to cardio-respiratory arrest
|
Slower disease progression
|
Rabies vaccination before a potential exposure primes the immune response so treatment after a suspected exposure can be effective more quickly.
Pre-exposure vaccination also reduces the number of vaccinations and simplifies treatment, should an exposure occur.
10